Many quality and patient safety leaders have multiple responsibilities within their departments. Wearing so many hats is a monumental challenge, but one that is made a bit easier by having the right tools available. Having worked with healthcare leaders in patient safety, quality, and risk for more than 25 years, we understand the challenge of feeling like sometimes you actually are the “I” in team.
American Data Network (ADN) has compiled a list of free resources that we hope can make your life easier and help you get more done in your pursuit of improving care at your organization.
Toolkits

Near misses represented only 6.8% of all 2016 events submitted to American DataNetworkPatient Safety Organization (ADNPSO), a representation significantly less than Unsafe Conditions or Incidents. Over one year, 45 hospitals dispersed across the state of Arkansas participated in ADNPSO’s Good Catch campaign. Overall, these hospitals achieved a 47% increase in near-miss reporting over baseline. Together, the participating facilities reported an average of 246 more near misses per MONTH during the campaign.
Moreover, the staying power of many of the organizations’ patient safety improvements was pretty dramatic. 63% of participating facilities reported a decrease in overall patient safety incidents [events reaching patients]. And they attribute that improvement to corrections and initiatives established in response to lessons learned through near-miss reporting.
Click here to read about the hospitals’ sustained results 6 months after the campaign.
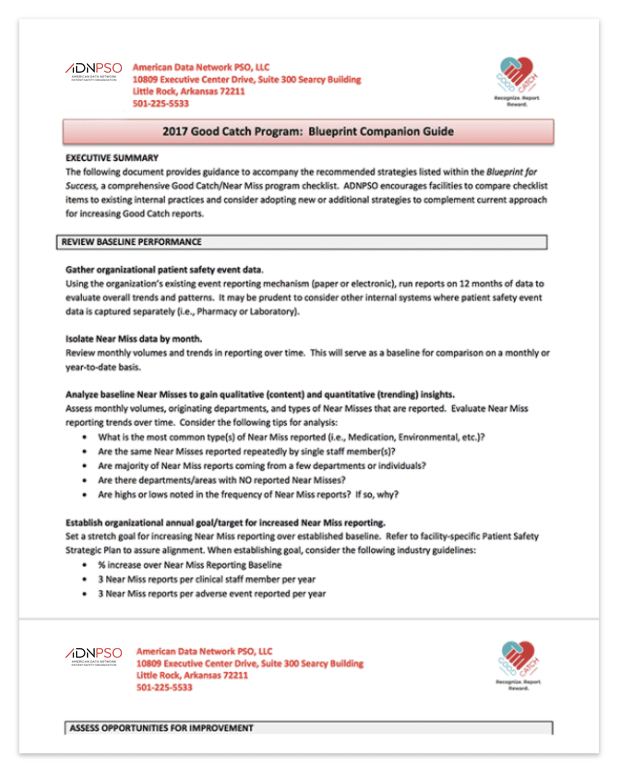
This robust toolkit provides the following and much more:
- Tips for Making the Most of Hospital Huddles (Video)
- Good Catch Program: Blueprint for Success
- Good Catch Program: Blueprint Companion Guide
- Good Catch Team Charter Document
- Good Catch Campaign References
- Good Catch Frontline Staff Education Powerpoint
Click here to download the Good Catch/Near Miss Campaign Toolkit
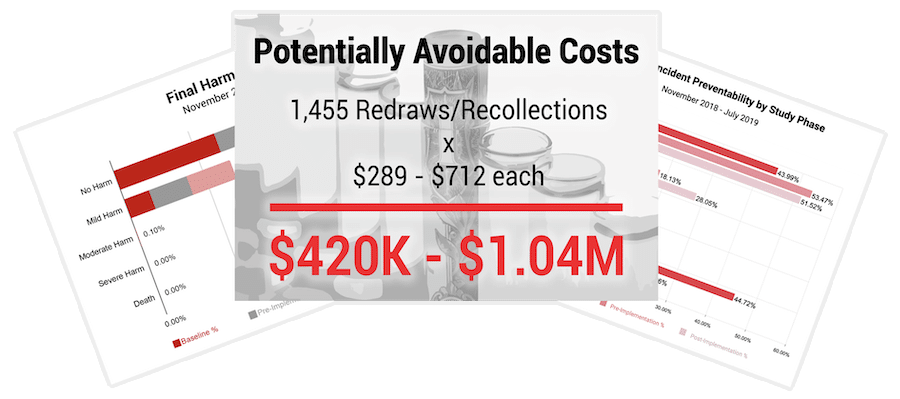
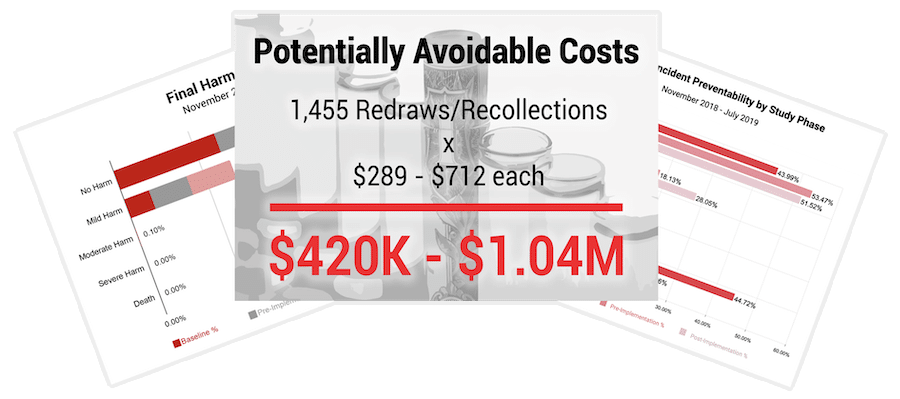
ADNPSO conducted a 9-month Specimen Focused Study in order to positively impact Patient Care, Satisfaction, Quality/Safety, and Finance. The study was designed to help healthcare professionals, both inside and outside the laboratory, better understand why specimen events happen and how they can collaborate to decrease errors across the testing process.
After analyzing 4 years of data, ADNPSO found specimen events consistently ranked among its highest reported errors with 73.7% of the incidents deemed preventable. ADNPSO participants realized a 147% increase in specimen event reporting during the study and potentially estimated avoidable costs of $420K – $1.04M – all in just 9 months.
This free toolkit is available for hospitals interested in running a similar Specimen Error Reduction Campaign.
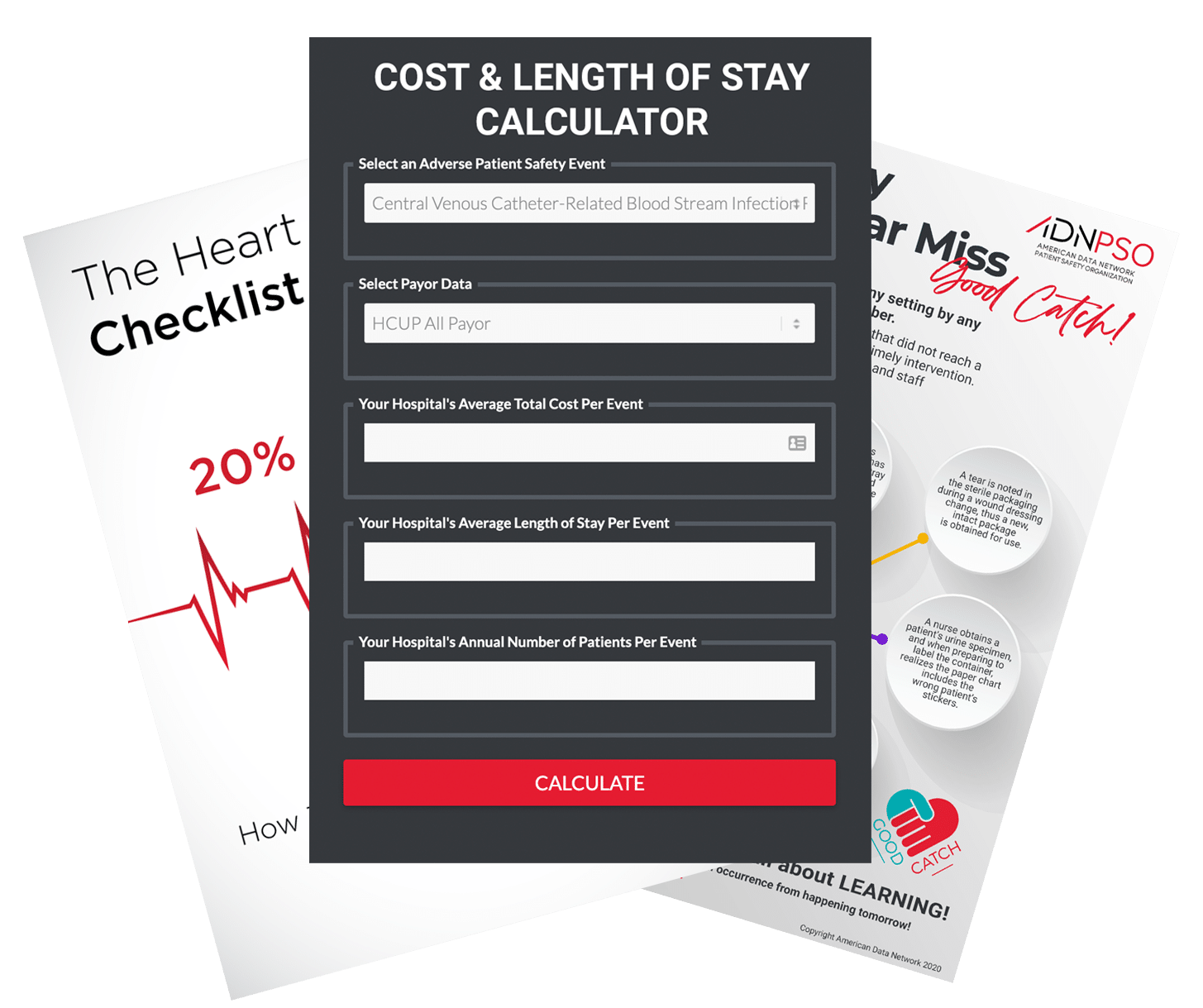
The Patient Safety & Risk Toolkit for Hospitals includes: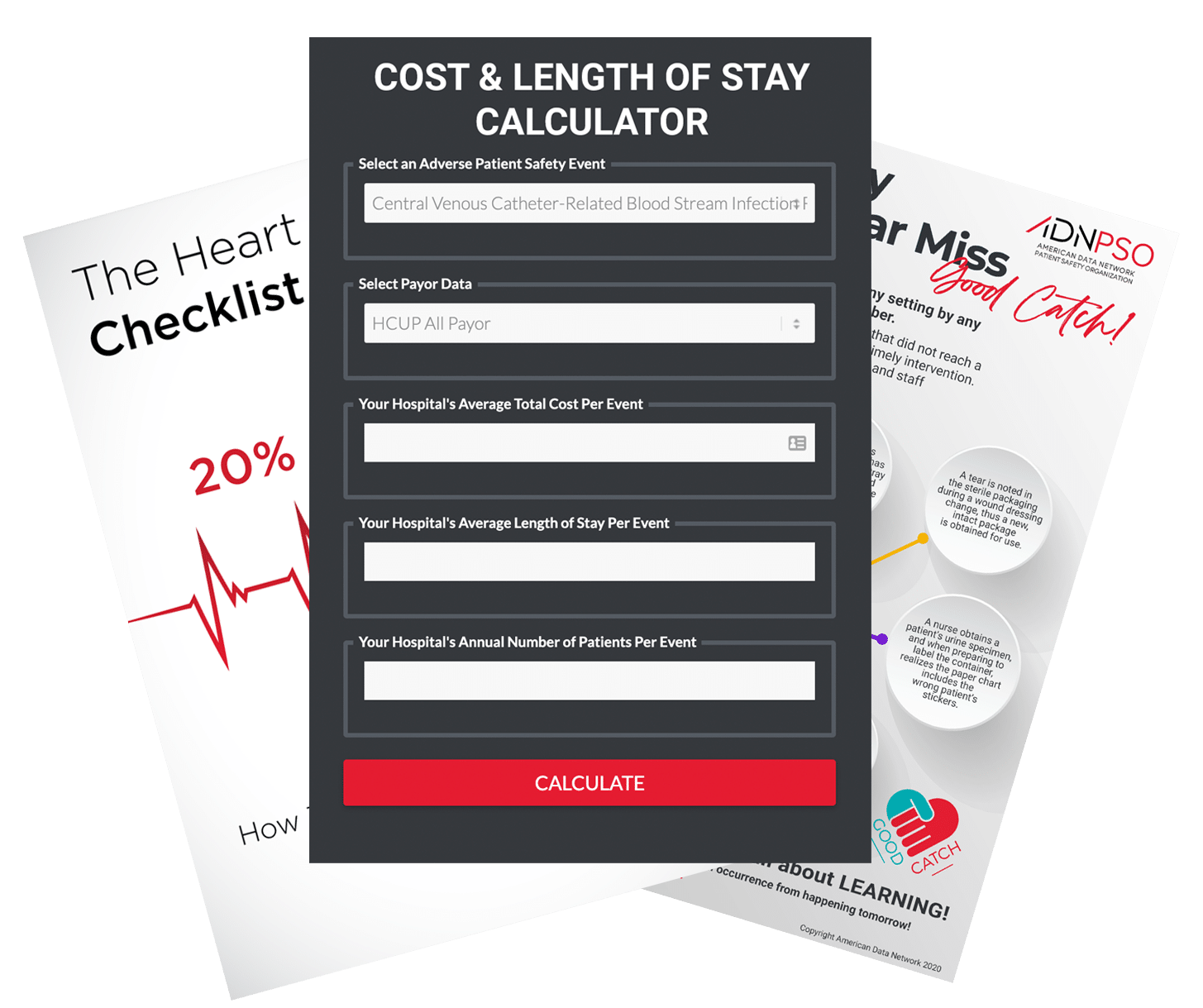
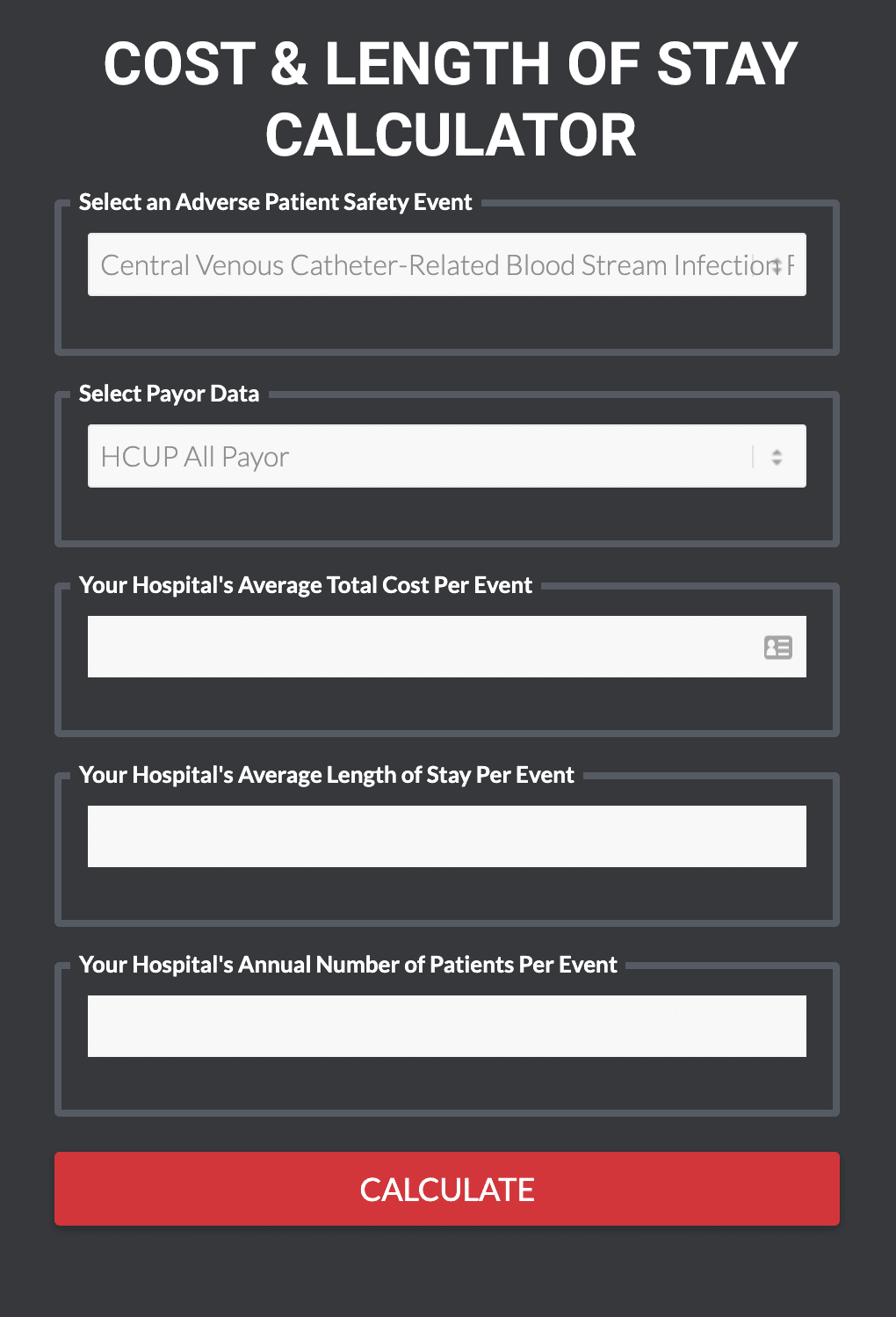
- Adverse Event Excess Cost & Length of Stay Calculator
- Good Catch Campaign Blueprint
- Heart Failure Checklist
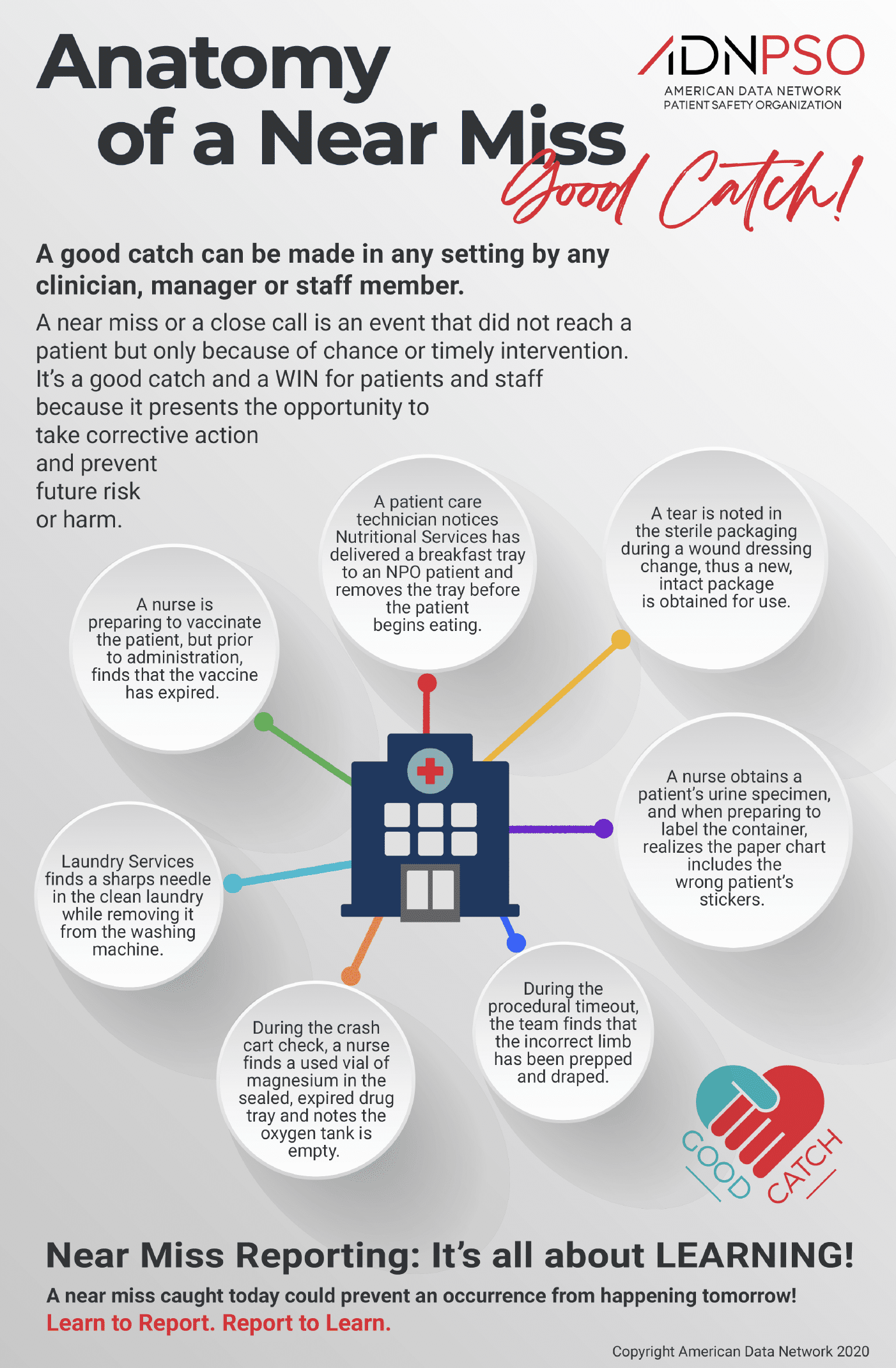
- Anatomy of a Near Miss Guide (Infographic)
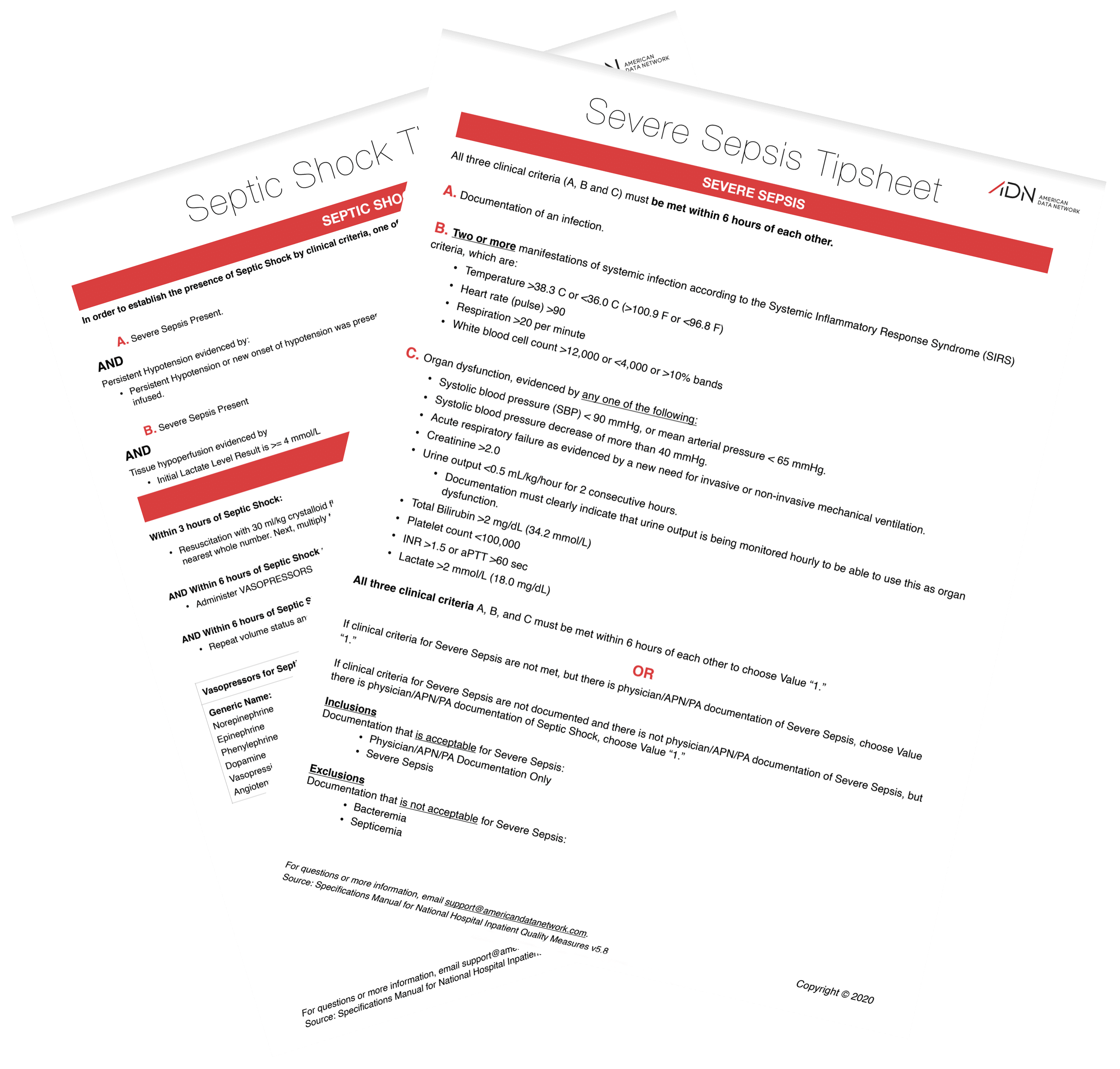
Tip Sheets
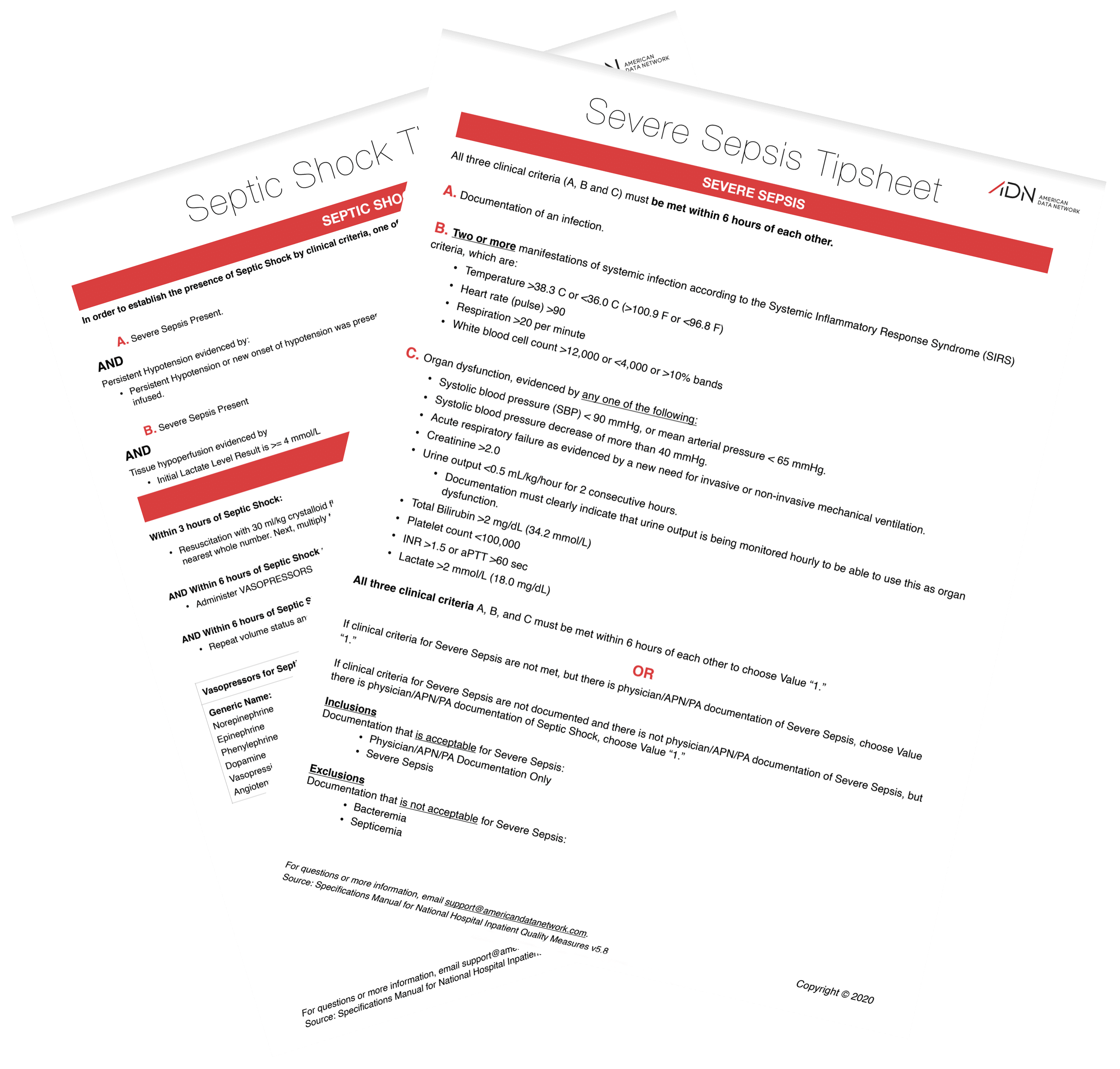
These are a set of straightforward checklists aimed at helping clinicians understand the defining criteria and suggested treatment protocols for Severe Sepsis and Septic Shock. These handy checklists can be downloaded, printed, laminated, and posted for quick reference by hospital staff.
Calculators
This Insourcing Cost-Benefit Analysis Template will enable you to make a data-driven decision on whether outsourcing is right for your facility.
Making the business case to senior leadership for an initiative or a new product or service can be difficult. This tool can help your team predict the return on investment of a patient safety or quality initiative that prevents a certain number of adverse events while also taking into account the soft cost of team time.
ADN has created a free calculator based on the Morse Fall Scale guide for a quicker and more efficient way to assess the risk factors of a patient falling.
Using this tool, medical personnel will:
- Quickly answer six short questions,
- Rapidly identify the likelihood of a fall,
- Estimate whether the risk is high, moderate, low, or if there is no fall risk present, and
- Use the final score to record it on the patient’s chart.
Predicting how your hospital’s improved performance will trend over time can be difficult and time-consuming.
Our team of data analysts and engineers built a free tool that allows you to forecast how improved performance will trend over time, using accurate prediction based on your historical data points.
With this free tool you can analyze:
- Average Cost Per Diagnosis
- Average Length of Stay
- Complications
- Core Measure Compliance
- Readmission Rate
- Mortality Rate
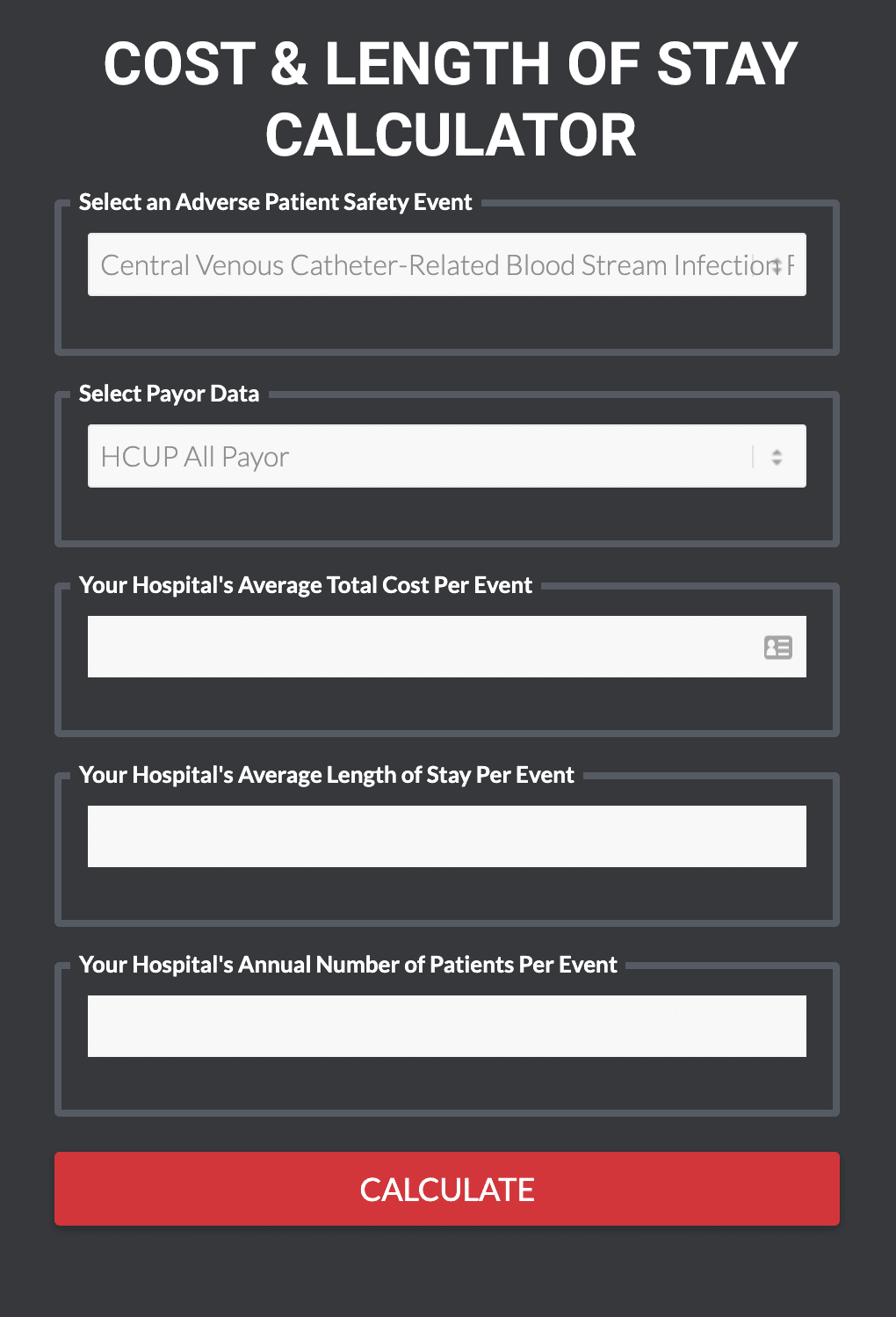
This calculator can assist facilities in quantifying their own excess cost and LOS for selectedPSIs simply by entering a few figures related to your own PSI volumes, cost and LOS.
Whitepapers & Study Research
 A Specimen Error is any defect that occurs during the entire testing process, from ordering tests to reporting results, and in any way influences the quality/safety of laboratory services. Tracking specimen errors to identify problems in the process is critical to patient safety as they can lead to injuries, misdiagnoses and delayed or unnecessary treatments. Every year American Data Network Patient Safety Organization (ADNPSO) identifies strategic initiatives to conduct in collaboration with its members.
A Specimen Error is any defect that occurs during the entire testing process, from ordering tests to reporting results, and in any way influences the quality/safety of laboratory services. Tracking specimen errors to identify problems in the process is critical to patient safety as they can lead to injuries, misdiagnoses and delayed or unnecessary treatments. Every year American Data Network Patient Safety Organization (ADNPSO) identifies strategic initiatives to conduct in collaboration with its members.
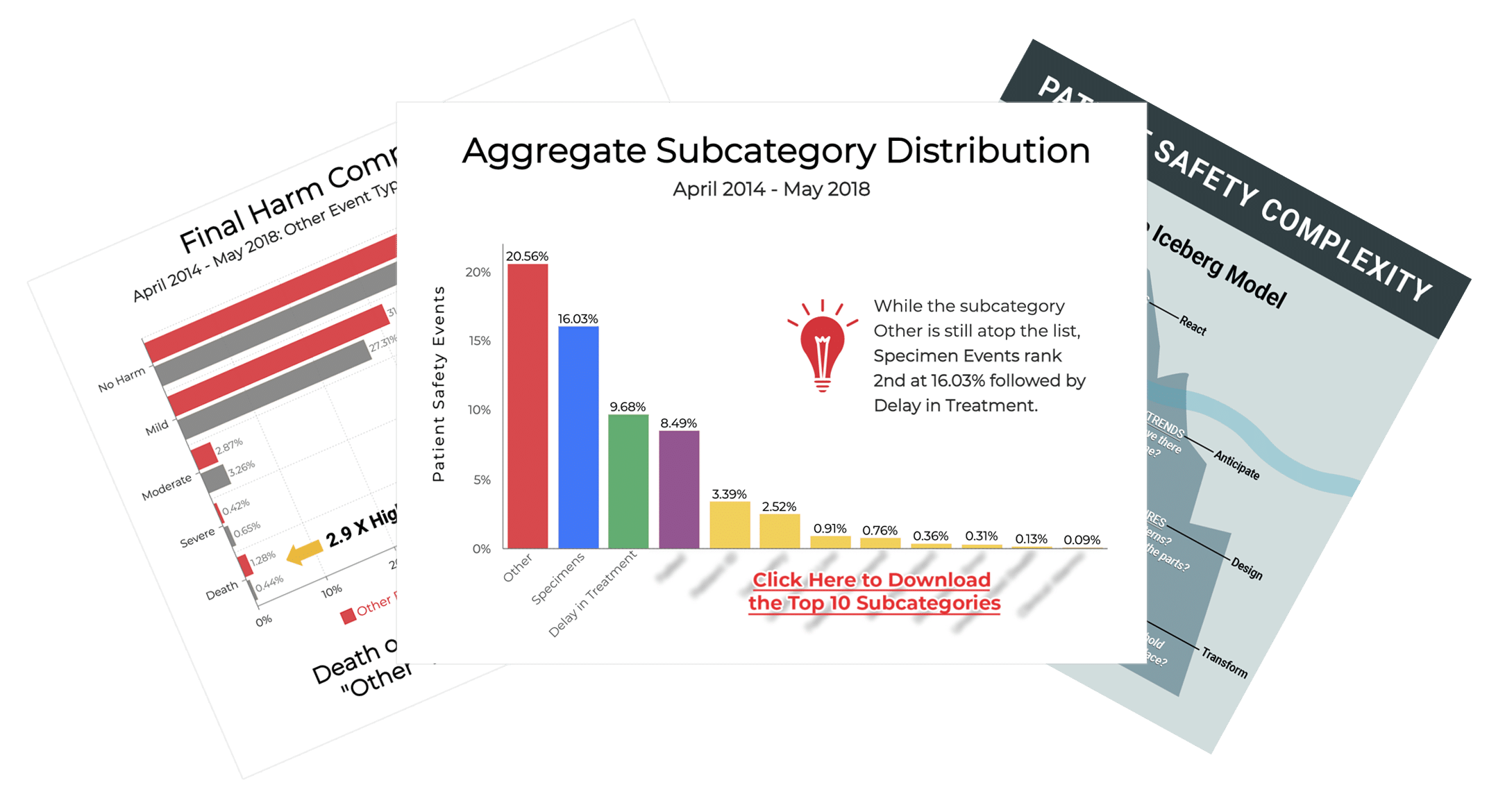
ADNPSO recognized the Other Event Type as a catchall category for errors that do not fit neatly into the standardized forms. During strategic planning, ADNPSO analyzed four years of Other event data, which revealed specimen errors ranked among the top reported subcategories.
Key Takeaways
- Specimen process awareness is key to propelling improvements.
- Redesign process steps to minimize risk for errors and distractions.
- A single event investigation can result in system-wide improvements.
- IT partnership and LIS optimization are essential.
- Successful education is designed to:
- Target roles/responsibilities specific to the staff levels involved.
- Provide rationale for standardized process steps.
- Include examples of how workarounds lead to negative outcomes in subsequent stages.
- Engineer change with persistence and reinforcement to create a new normal.
 ADNPSO collaborated with Patient Safety and Laboratory experts to create a specimen data collection form and recruited PSO members to join the study. In partnership with the 15 acute care participants, ADNPSO performed aggregate analytics, hosted learning sessions to discuss findings, guided Rapid Cycle PDSAs, and developed detailed Process/Cause Mappings to galvanize improvement activities.
ADNPSO collaborated with Patient Safety and Laboratory experts to create a specimen data collection form and recruited PSO members to join the study. In partnership with the 15 acute care participants, ADNPSO performed aggregate analytics, hosted learning sessions to discuss findings, guided Rapid Cycle PDSAs, and developed detailed Process/Cause Mappings to galvanize improvement activities.
In this webinar, we’ll discuss:
- The results of the study, including error trends,
- Real-world improvements that the participating hospitals made, and
- The financial impact of the potentially avoidable costs.
In 2018, ADNPSO conducted a deep-dive analysis of the event type “Other.” Over a four-year period, this catchall category accounted for over 40% of events reported by ADNPSO members. Among the myriad of striking revelations, the death rate of incidents categorized as Other was 3 times higher than ALL remaining event categories combined. The results of the Other analysis proved so compelling that ADNPSO was selected to present at the National Association for Healthcare Quality (NAHQ) Next Conference in November 2018. The findings underscore the valuable insight buried in the Other event category.
Key Takeaways
- The biggest takeaway was uncovering the incredible potential hidden in the event type Other. This is very important considering these events could have a mortality rate 3X higher than all remaining event types combined.
- Time should be made by Patient Safety and Risk Managers to review and recategorize Other events before they are closed and used in analytics reports to ensure teams are focusing on an accurate set of priorities.
- Organizations may be missing analytic opportunities for spotting key trends in patient safety data if using paper processes, EHR add-on modules or in-house built databases to collect events. Not to mention, the significant time spent to manually enter events and build meaningful reports; time that could be reallocated to analysis and improvement efforts.
This study also includes suggested action items to help identify what is hidden in your organization’s Other event type.
Case Studies, eBooks, & Guides
“How 45 Hospitals Increased Near Miss Reports by 47% Plus A Guide to Run the Same Near MissCampaign”
While experts consider near misses to be unmatched predictors of medical error, research shows they are markedly underreported. ADNPSO data confirmed that notion. Near misses represented only 6.8% of all 2016 events submitted to ADNPSO, a representation significantly less than Unsafe Conditions or Incidents.
As a commitment to caring for and keeping patients safe, it is critical that we evaluate and learn from every event reported, including those where no patient harm resulted. Leadership responsibility includes assurance that staff recognize all types of events and are supported in their reporting activities.
In this ebook, we discuss:
- What staff needs to be trained on,
- Examples of patient safety events and near misses, and
- A Leadership To-Do List
With the ever-increasing demand for healthcare quality data, it is essential that organizations produce data that is complete, valid, and reliable.
In this ebook, we discuss:
- What Inter-rater Reliability is,
- How to do it, and
- Why your hospital’s bottom line is at risk without it.
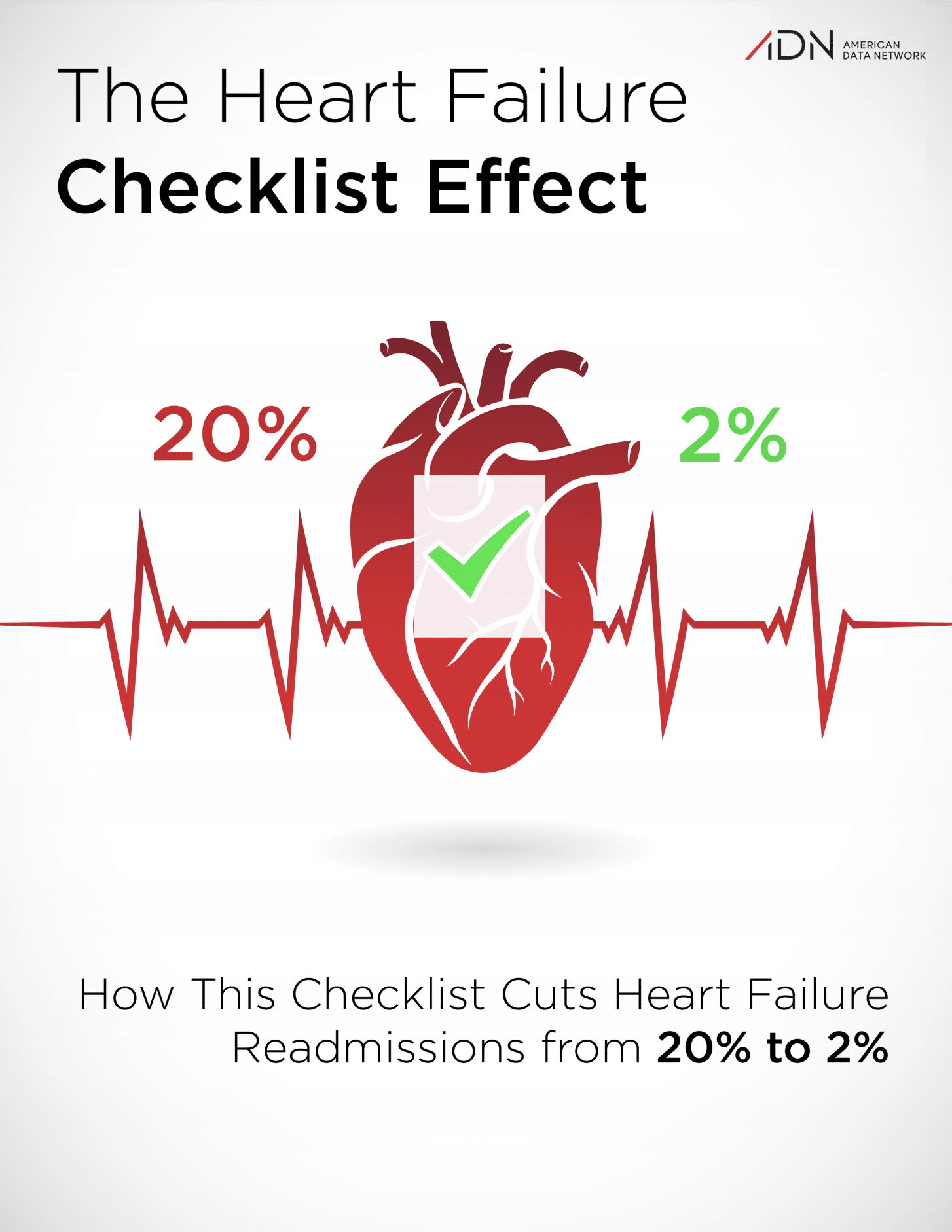
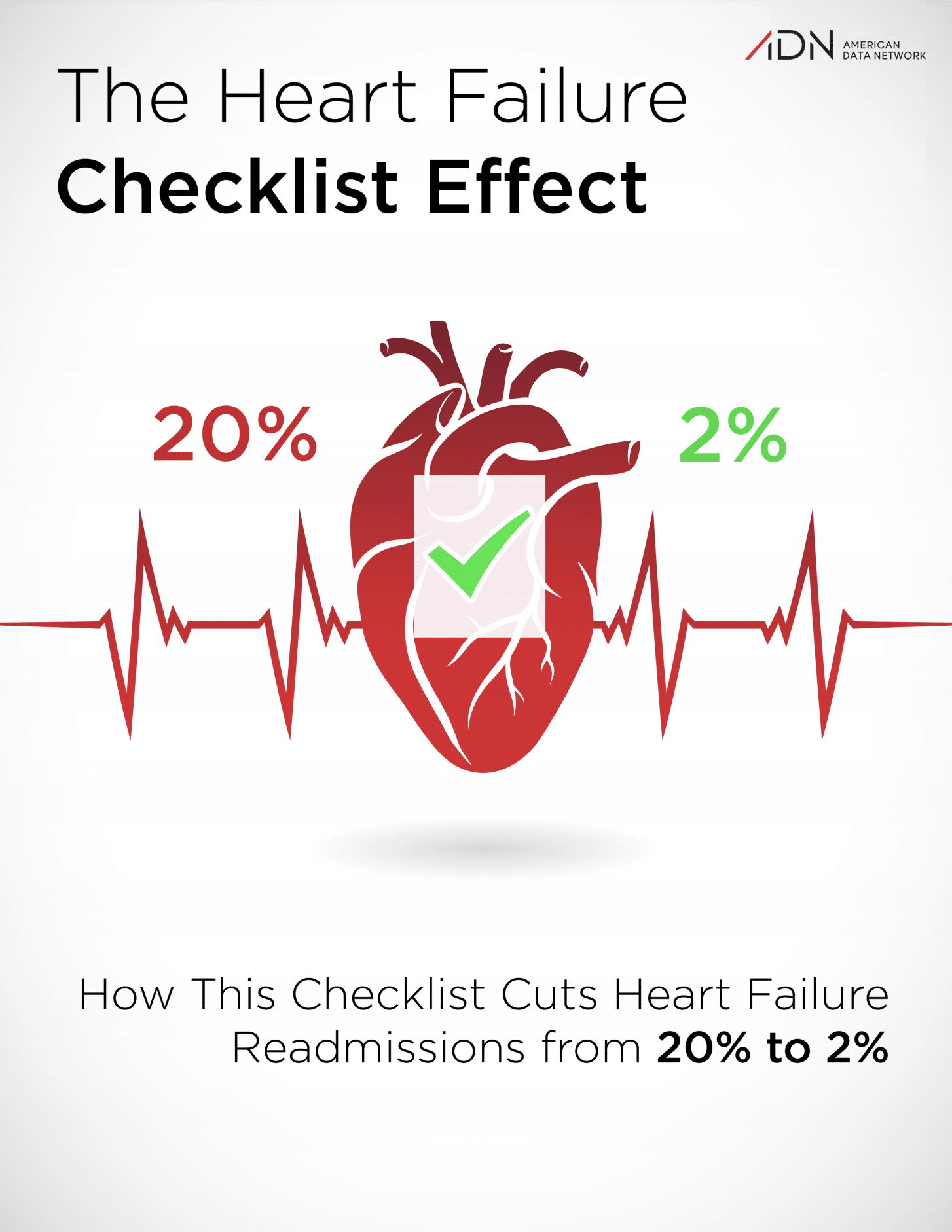
Research conducted at St. Joseph Mercy Oakland Hospital and presented at the American College of Cardiology’s 61st Annual Scientific Session has shown that the use of a 27-question, heart failure discharge checklist reduced the 30-day readmission rate of a cardiac event from 20 percent to only 2 percent.
The checklist is divided into three sections:
- Medications and appropriate dose modification,
- Counseling and monitoring intervention, and
- Follow-up instructions.
To ensure a thorough analysis of event data, multiple reports should be compared and contrasted in order to unveil additional hidden contributing factors for improvement priorities. These are the Top 5 Reports every patient safety and risk department should be building to get the best insight into their data.
ADN has published a business case titled “A Business Case: Identifying Excess Cost & Length of Stay of Adverse Patient Safety Events” using the Agency for Healthcare Research and Quality’s (AHRQ) Patient Safety Indicators (PSI)
to evaluate excess cost and Length of Stay (LOS) per type of adverse event. The data used was benchmarked against both the HCUP All Payer database (4+ million records representing 484 facilities) and the CMS MEDPAR database (13+ million records representing 3,378 facilities).
ADNPSO organized a statewide Good Catch Campaign in Arkansas in 2017. Using this GoodCatch Campaign Blueprint, along with other materials provided by ADN in the Good Catch Toolkit, 36 facilities reported nearly 10,000 Good Catches. Some facilities even noted their Good Catches improved more than 30%. This blueprint can be downloaded for free so your facility can continue its work to improve patient safety and healthcare quality.
Videos

This video is designed to help hospital staff build and manage an effective huddle system that perpetuates timely, thorough communication regarding patient and staff safety issues organization-wide.

ADNPSO’s 90-Second Post Fall Assessment video can be used as an educational tool to guide nurses toward an overall initial impression in determining the cause of a fall and establishing priorities for patient care interventions and prevention of repeat falls.
Most healthcare organizations are heavily invested in data collection, yet their efforts are fragmented across administrative and clinical roles. A comprehensive, system-wide data inventory allows organizations to improve and streamline collection by identifying disparate data sources, responsible staff, reporting requirements, and regulatory implications.
Posters/Infographics
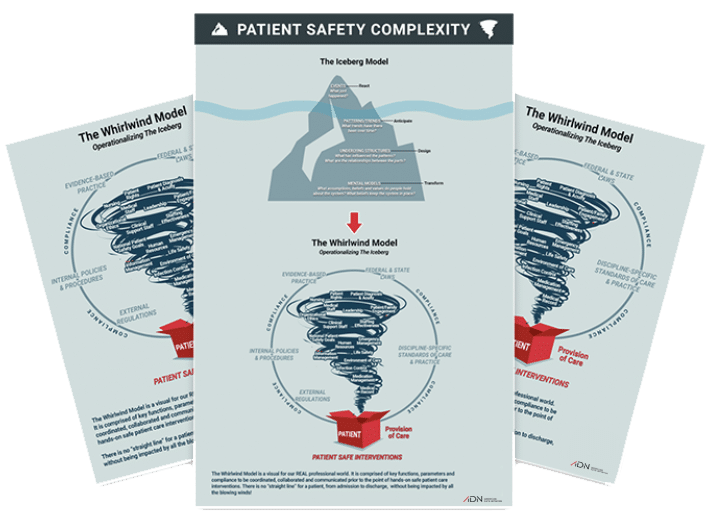
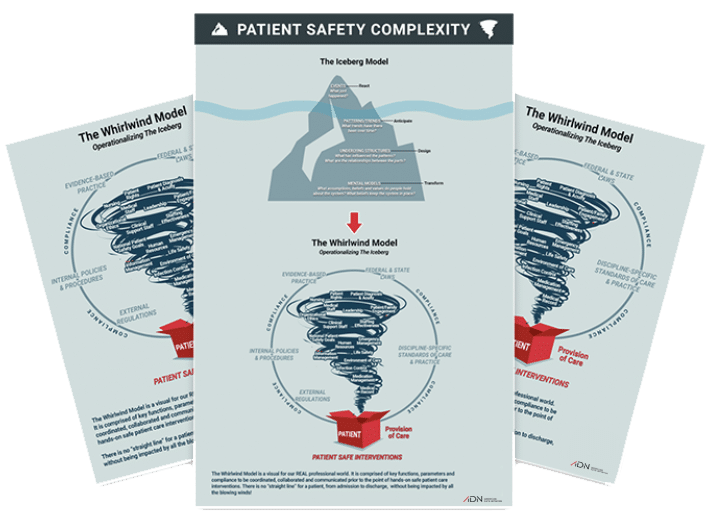
The iceberg model has been used in health care to illustrate that many times much bigger things beneath the surface contribute to patient safety events. The incidents are what we see on the surface of the iceberg but beneath that surface are near misses and the unsafe conditions that cause them. The iceberg model takes analysis from the occurring incident down to identifying patterns and trends, to discovering what influenced those patterns and trends, and to identifying the assumptions and beliefs that are keeping the system in place.
By flipping the “Iceberg” model upside down we created the “Whirlwind Model” in order to operationalize it. The WhirlWind Model illustrates the key functions, parameters, and compliance efforts that must be coordinated, collaborated, and communicated in order to deliver safe patient care.
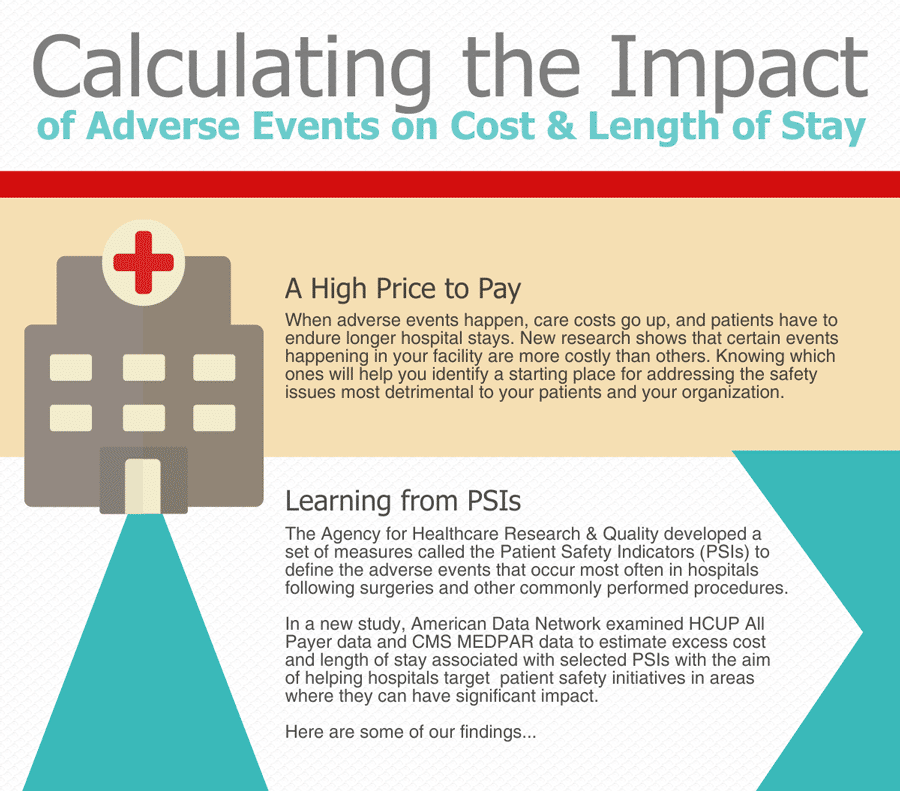
ADN has published a business case titled “A Business Case: Identifying Excess Cost &Length of Stay of Adverse Patient Safety Events” using the Agency for Healthcare Research and Quality’s (AHRQ) Patient Safety Indicators (PSI) to evaluate excess cost and Length of Stay (LOS) per type of adverse event.
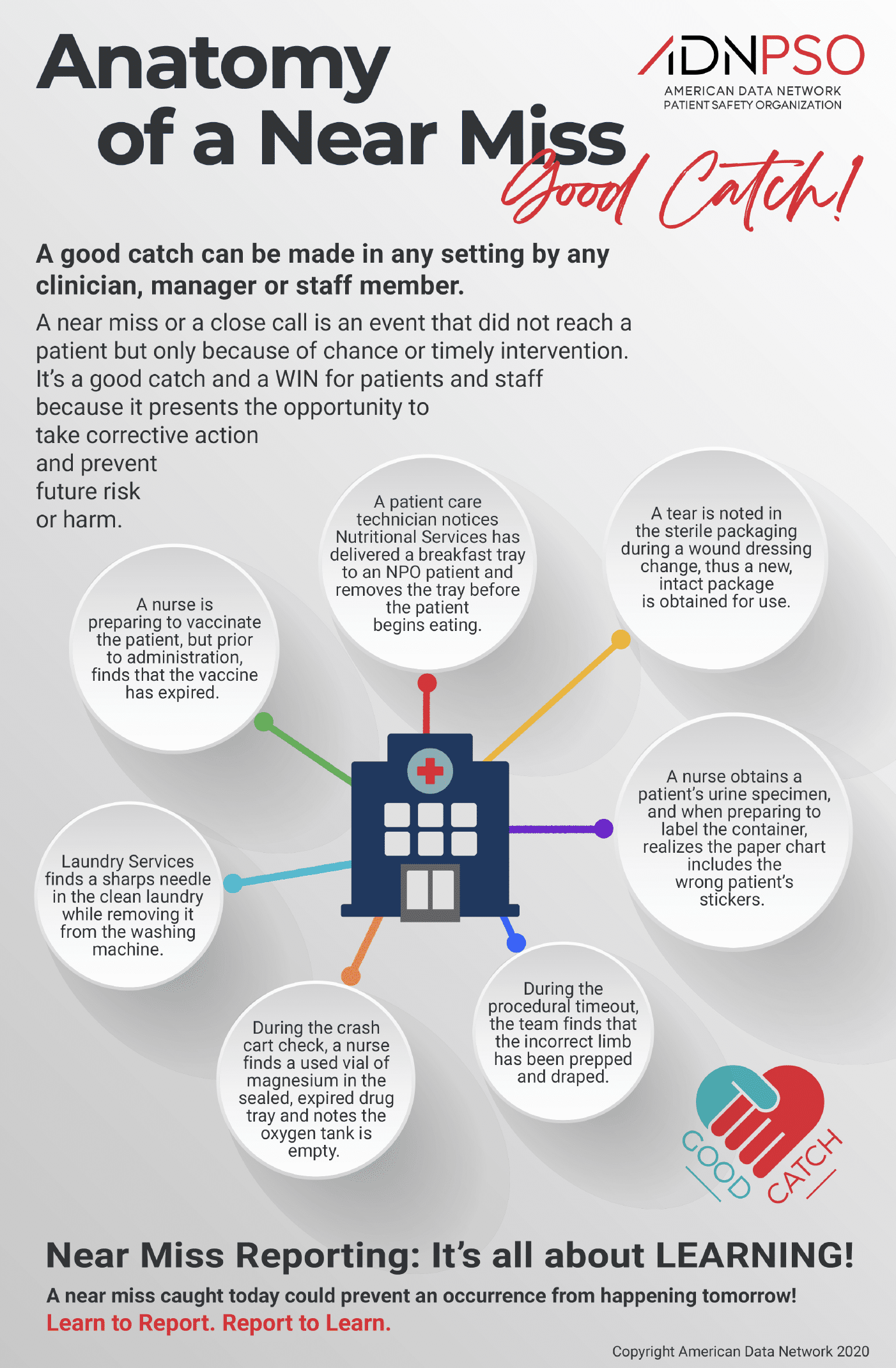
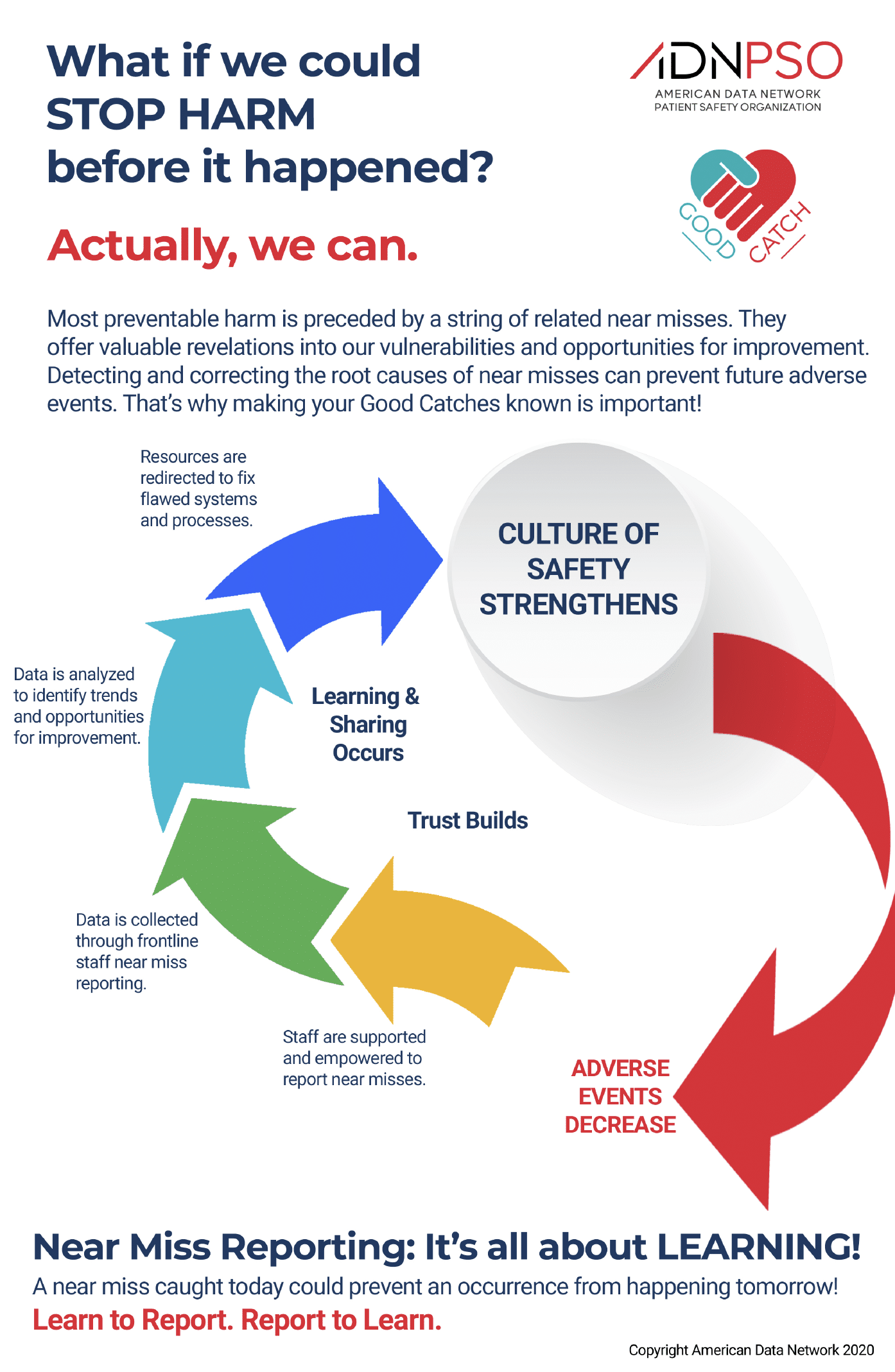
A near miss or a close call is an event that did not reach the patient but only because of chance or timely intervention. It’s a Good Catch and a WIN for patients, staff, and hospitals because it presents the opportunity to take corrective action or prevent future risk or harm. A near miss caught today could prevent an occurrence from happening tomorrow.
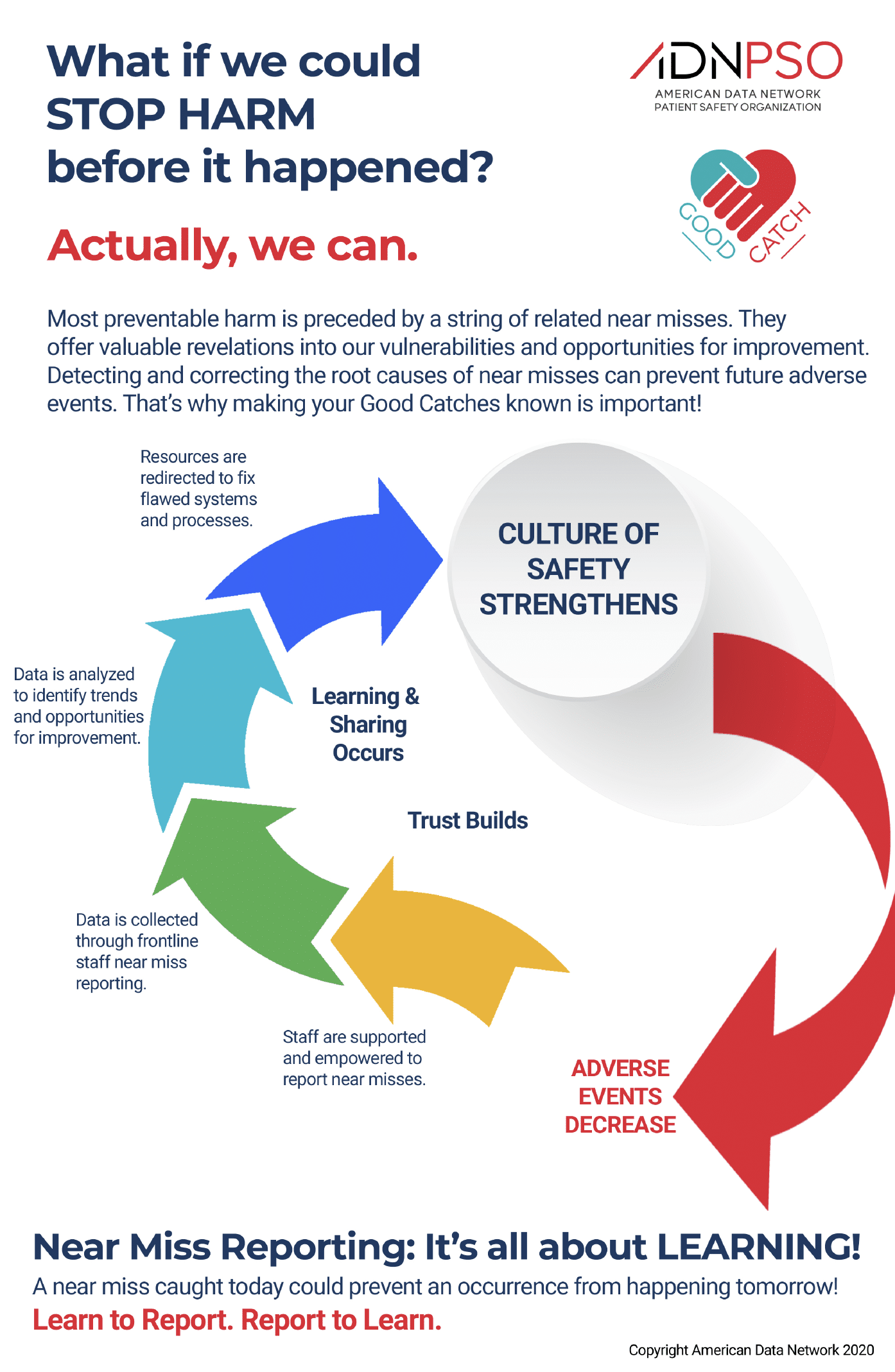
Most preventable harm is preceded by a string of related near misses. These close calls are free lessons. They offer valuable revelations of our weaknesses AND strengths – our opportunities for improvement. That’s why making your Good Catches known is so important!
For more than 25 years, American Data Network (ADN), which is also the parent company to its Patient Safety Organization (ADNPSO), has worked with large data sets from various sources, aggregating and mining data to identify patterns, trends, and priorities within the clinical, financial, quality and patient safety arenas. ADN developed the Quality Assurance Communication (QAC) application, with which hospitals, clinics, rehabs, and other providers record and manage patient safety events. By entering events into ADN’s QAC application and submitting them to ADNPSO, information is federally protected and thereby privileged and confidential. These protections provide a safe harbor to learn from mistakes and improve patient safety.