What is voluntary patient safety event reporting?
Voluntary event reporting is the process of collecting details about an incident, near miss, or unsafe condition in hospitals or other care settings. This information is typically submitted by frontline staff through an electronic or paper-based form. Implementing effective reporting systems can help hospitals prevent future events.
Table of Contents
- Understanding Why Reporting Often Fails
- Strategies for Encouraging Voluntary Event Reporting
- Regular Education and Reinforcement
- Provide Feedback and Show Results
- Create Convenient and Natural Reporting Opportunities
- Leadership Encouragement
- Recognition and Rewards
- Intensive Reporting Days
- Tracking Progress
- Building a Culture of Transparency
As research published by the Journal of Patient Safety in 2020 acknowledged, “A natural, human tendency when errors have occurred is to ignore or minimize the error. It takes a lot of work to build an environment that supports the opposite reaction: open and honest reporting of errors so they can be evaluated to contribute to organizational learning.”
Although counterintuitive, embracing failure is crucial for achieving high reliability. Organizations must defy human nature by eagerly embracing the evidence of failure. This article will suggest six strategies, and even more specific techniques, for creating a culture that encourages — and even incentivizes — team members at all levels to report incidents, near misses and unsafe conditions. To further understand these processes, explore our patient safety event reporting guide.
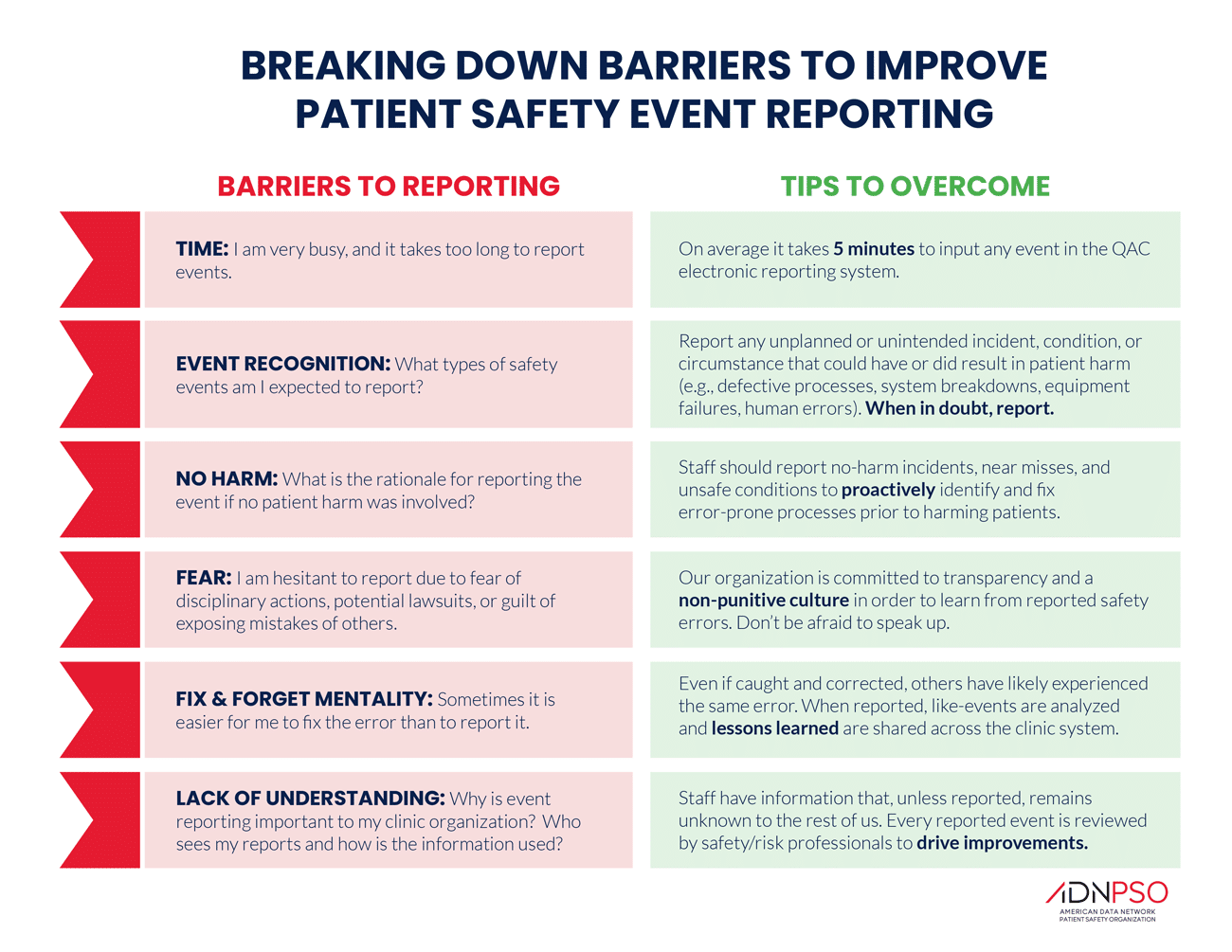
Understanding Why Reporting Often Fails
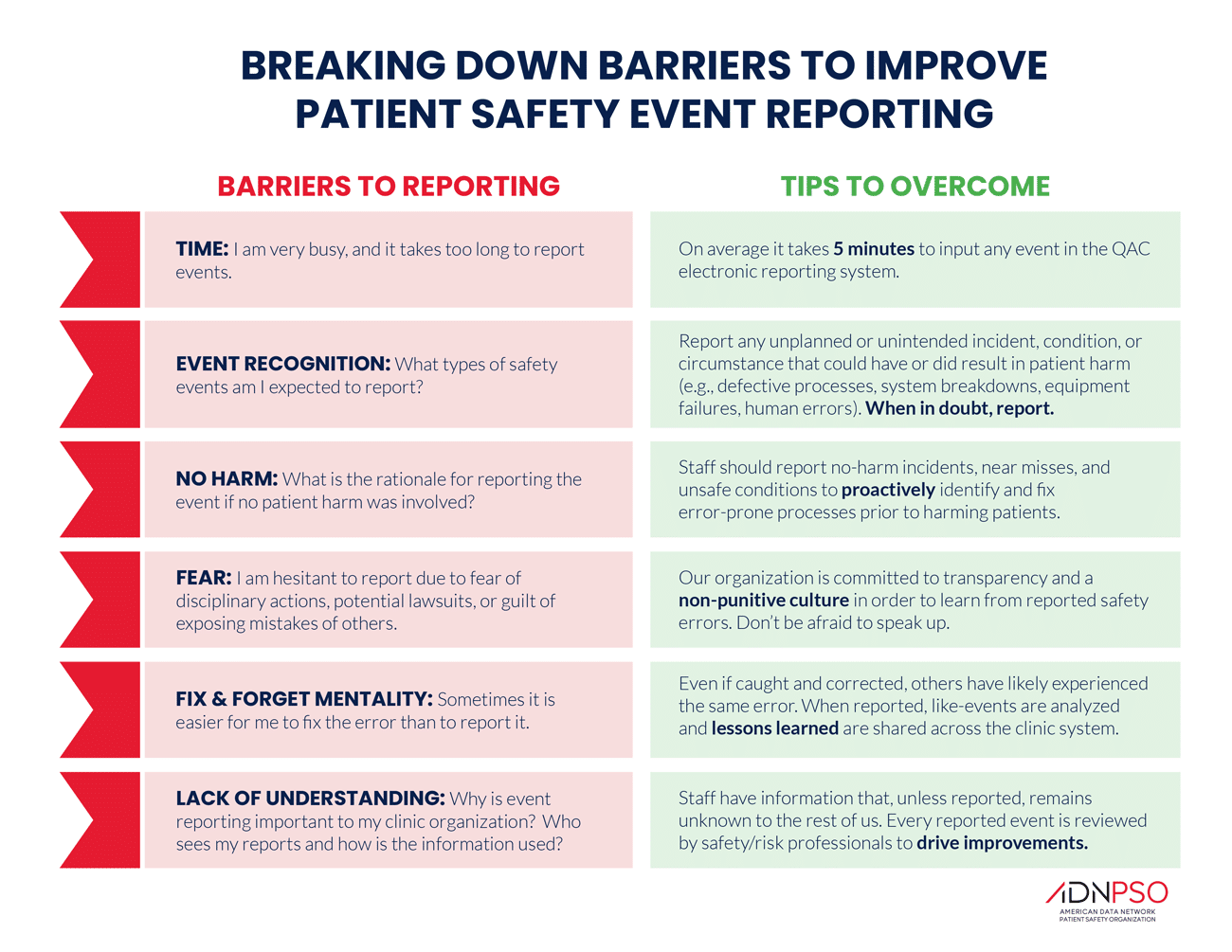
Encouraging reporting starts by understanding why staff might hesitate – as the graphic below illustrates.
Team members must understand the big picture – preventing future patient safety events by analyzing and sharing past errors. Preoccupation with failure is a mindset that must be fostered at every level. Reporting of safety events and concerns must be recognized as a critical component of patient care.
Team members also must be assured that reporting will not create problems — for themselves, their coworkers or the facility. Fear of immediate personal repercussions is a disincentive to future patient safety. If you want to trust your staff to report safety concerns and events, your staff must trust that they will not regret reporting. Snitches prevent stitches!
Strategies for Encouraging Voluntary Event Reporting
-
Regular Education and Reinforcement
Awareness of patient safety as a science has grown, but your hospital or clinic is an amalgam of patient care providers whose immersion in the mindset and culture of patient safety cannot be assumed. Your facility’s safety culture and processes for reporting issues must be central to the onboarding and orientation process. Reinforce these concepts through continuous training to normalize voluntary event reporting.
As Susan Trossman noted in The American Nurse (2017), cultural expectations like engaging in daily safety huddles and collaborative work must be communicated to new hires and reinforced in continuing training and routine communication. Intensive orientations – especially for nurses – have the added benefit of improving staff retention.
Appointing safety champions – engaged team members with specialized training – in each department is a proven way to normalize the routine reporting events. These champions can ensure the focus on voluntary event reporting remains a priority.
-
Provide Feedback and Show Results
Showing staff that their reports lead to real improvements creates a feedback loop: reporting leads to changes, which encourages more reporting. An analysis of data from more than 200,000 individuals in almost 1,000 hospitals concluded that prioritizing feedback to reporters is one of the most efficient ways to increase voluntary event reporting. This was especially true with the most serious patient safety events.
Using terms like “safety report” instead of “incident report” can also shift the focus from blame to improvement.
-
Create Convenient and Natural Reporting Opportunities
You may be familiar with “nudge theory,” which suggests that making desired behaviors more convenient encourages people to follow through. This concept can be applied to voluntary event reporting by creating convenient, natural opportunities for staff to report incidents.
One common and effective strategy is the daily huddle, in which patient safety is the central agenda item for all team members. Periodic observation to make sure daily huddles are being used to encourage event and near-miss reporting is a good management technique. Try adding the daily question: “How is the next patient going to be harmed?” to maintain an ongoing focus on safety.
Since time and effort are often barriers, user-friendly reporting technology can further nudge behavior. Tools like our patient safety event reporting application simplify the reporting process. To evaluate your current system, use our free Patient Safety Event Reporting Gap Analysis template, which helps identify improvements in your event reporting process.
-
Leadership Encouragement
Support from leadership is crucial for fostering a culture of voluntary event reporting. When leadership promotes reporting, it dispels the fear of retribution and encourages a just culture. ADN’s Increase Event Reporting Toolkit offers templates for emails from senior leaders to help communicate this message effectively. Additionally, hanging posters reminding frontline staffers of the types of events they should report can keep the responsibility for reporting top of mind. You can also explore more strategies in our national patient safety goals guide.
Every communication channel – staff meetings, intranet, newsletters – can reinforce the importance of reporting. However, ensuring someone is specifically responsible for safety communication is key. Voluntary reporting should become a standing item on meeting agendas to guarantee consistent attention.
-
Recognition and Rewards
Behavior rewarded is behavior repeated. Recognizing voluntary event reporting through “good-catch campaigns” motivates staff to continue reporting. Rewards can include certificates, plaques, or even a paid day off for the staff member who reports the best good catch each quarter.
If your state has a patient safety recognition program, ensure your good catches are submitted. Whether or not the staff is recognized statewide, the acknowledgement reinforces their focus on safety.

-
Intensive Reporting Days
While voluntary event reporting is encouraged year-round, designating Intensive Reporting Days can significantly increase reporting. Research published in the Journal of Patient Safety found this technique effective across all organizational levels, especially when reporting is made conveniently and anonymously.
Clinicians, staff members and patients in 10 family medicine clinics were encouraged to make routine reports during a 10-week study, but they were asked to report every error on five specific days. Their anonymous reports could come through a website, paper forms or a voice-activated phone system. During the 70-day study period, more than a third of the reports came on the five days that were designated for intensive reporting.
ADN’s Increase Event Reporting Toolkit offers an Intensive Reporting Day checklist and support materials to help your organization implement this proven strategy for increasing voluntary event reporting
Tracking Progress
As you implement new strategies and techniques to improve voluntary event reporting, tracking progress is essential. ADN’s Patient Safety Event Reporting Rate Calculator allows you to measure overall improvement and compare your facility’s performance to others. The calculator provides insights into how your event reporting rate stacks up against the average, along with suggested goals and tailored strategies for further improvement.
Building a Culture of Transparency
By embracing these strategies, your organization can foster a culture of transparency where voluntary event reporting becomes second nature. Encouraging staff to report incidents, near misses, and unsafe conditions not only improves patient safety but also strengthens overall care quality. With tools like ADN’s Patient Safety Event Reporting Application and resources like the Increase Event Reporting Toolkit, you can track your progress and continually refine your approach. Creating a safer environment for patients starts with a commitment to voluntary event reporting – an essential step toward achieving high-reliability healthcare.
You May Also Like: